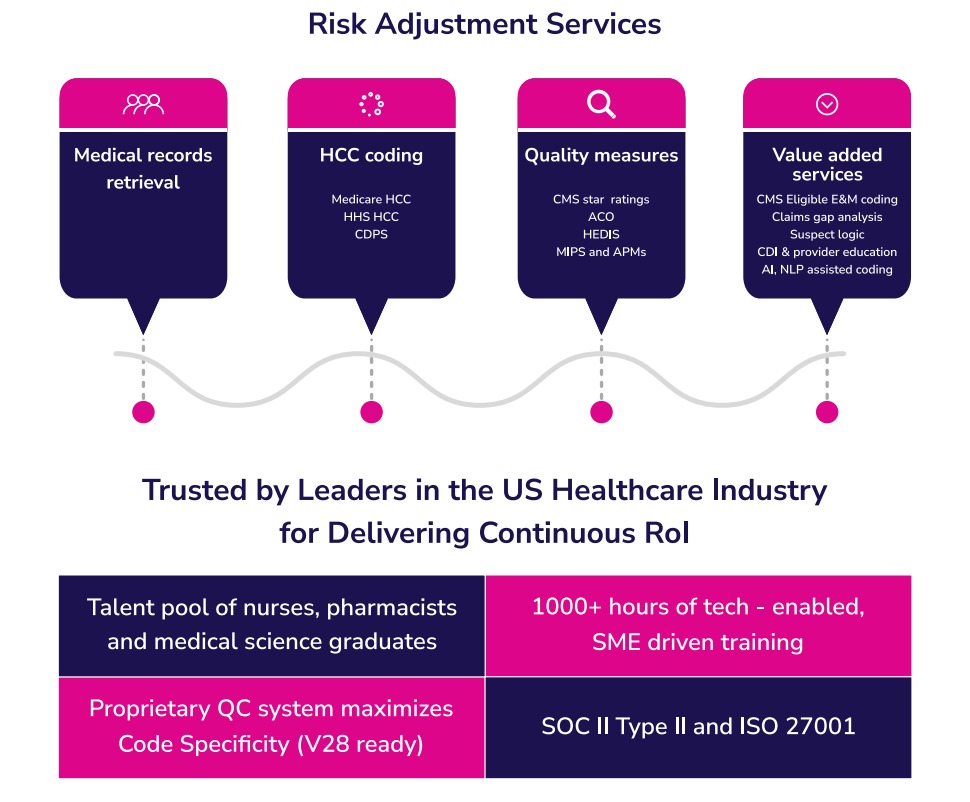
Data, Tech & Risk Adjustment Expertise
We are a Human-in-the-Loop BPM 4.0 company leveraging four core pillars – Data & Tech, Risk Adjustment Expertise, Security &
Compliance and Talent Innovation — to deliver continuous Rol to clients. We have the expertise, experience, talent plus that ability to scale. We have a record of exceeding client metrics and we have demonstrated that we just do better.

The Compliance team at Annova approaches projects from three key perspectives: CMS, Payer’s standpoint, and Vendor’s viewpoint.

Compliance and High Quality Coding Practices
CMS
While it may seem that RADV audits are focused on HCC conditions which have often been associated with inappropriate high-risk scores, inadequate documentation and fraud, there is a broader focus. CMS aims to drive payers and providers toward Patient wellness and disease prevention, emphasizing its reflection in documentation. For instance, comparing the documentation of “Breast cancer followed up by the oncologist” to “Breast Cancer, following up with oncology for hormonal chemo options, monitoring benefit vs risk due to osteopenia and history of falls” reveals the latter’s holistic patient management approach. In contrast, the former raises doubts about the actual presence of cancer. CMS strives for patient management beyond risk scoring and documentation concerns.
PAYORS
Payors want to prevent CMS rejections and costly retrospective reviews by expecting providers to accurately document risk-adjusted conditions to facilitate precise risk score calculation. Even though payers understand the risk of RADV audit and the interconnectedness of comprehensive patient care and proper documentation, this synergy is not consistently reflected in project guidelines provided to coding vendors. Despite the risk of rejections, conditions are often coded without active MEAT and from past headers. High-risk conditions such as cancers, fractures, and CVAs are frequently documented without sufficient active evidence due to outdated or inaccurately interpreted guidelines.
Vendors
Vendors frequently prioritize steering clear of errors identified in coding audits conducted by payers (in-house or third-party auditors). Their attention tends to center on administrative details such as provider NPI, place of service, and signature issues, rather than addressing the broader goal of accurately coding risk-adjusted conditions to the highest specificity and identifying documentation deficiencies.

Solutions
The compliance team identifies high-risk coding practices within teams, investigates the root causes, and provides solutions with the core objective of safeguarding the interests of the payer. Annova’s compliance team, consisting of experienced risk adjustment coders and compliance experts, collaborates with Clients/payers, their coding teams and Annova’s in-house coders. The team’s primary focus is on working with clients on creating and updating reference and training documents in alignment with recent changes, CMS findings, and emerging risk adjustment coding trends. The team helps strengthen the audit process by focusing on the areas that matter, helps coding teams to interpret the project guidelines and focus on accurate coding.

